DIEP Flap Breast Surgery
The DIEP flap (Deep Inferior Epigastric Perforator) is a technique utilized in reconstructive breast surgery, after removal of a whole breast (mastectomy/bilateral[double] mastectomy) or part of the breast (segmental mastectomy, quadrantectomy) or part of the breast (segmental mastectomy, quadrantectomy or wide local excision), whereby the lower abdominal skin and fat are transplanted to rebuild the breast(s). The DIEP flap is one of the most advanced operations for breast reconstruction and patients have experienced significant enhancement in their quality of life and return to normalcy thanks to the natural results, as well as an improvement in abdominal contour achieved by Dr. Rad.
Dr. Rad is considered one of the premier physicians in DIEP flap reconstruction. Dr. Rad works diligently with you to ensure your goals for symmetry, size and proportion are reached. Having performed hundreds of DIEP flap operations, Dr. Rad’s success rate exceeds 99% and his patients enjoy quick, comfortable recovery as well as results that last a lifetime.
In Dr. Rad’s hands, the DIEP Flap is the perfect option for patients who:
- have plentiful abdominal fat
- do not want, or can not have (due to radiation treatment), implant reconstruction
- want their breasts to be rebuilt with their own healthy tissue
- want to be finished with surgery forever (this cannot be said for implant reconstruction)
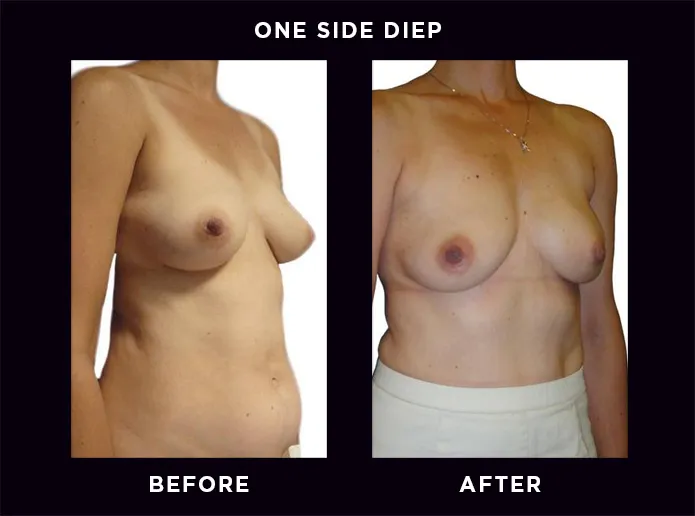
DIEP Flap: one side DIEP
- The DIEP flap is ideal for one-sided reconstruction for both nipple-sparing and non-nipple sparing mastectomy.
- An inframammary (under fold) scar placement is ideal to hide the evidence of mastectomy.
- Dr. Rad endeavors to render the scar invisible and patients can appear never to have had surgery.
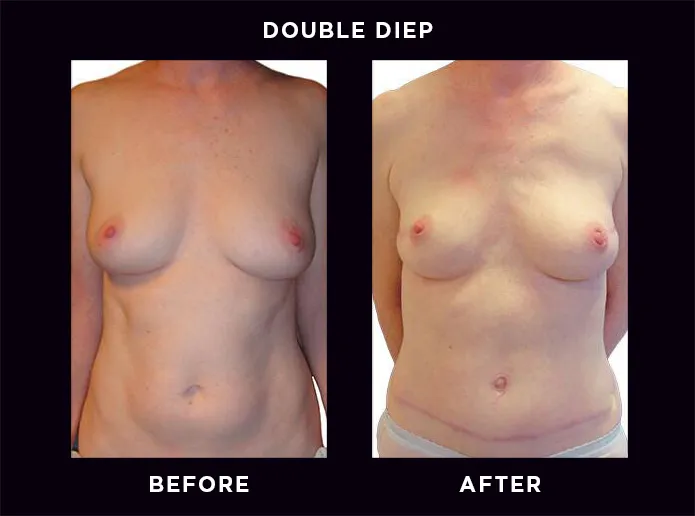
DIEP Flap: double DIEP
- Bilateral reconstruction with the DIEP flap is Dr. Rad’s preferred method when there is plentiful abdominal tissue.
- Dr. Rad endeavors to render the scar invisible and patients can appear never to have had surgery.
DIEP Flap: BRCA Gene
- Angelina Jolie carries the BRCA1 gene. With this gene, she had a 45% chance of developing breast cancer by age 70. She chose a preventive double mastectomy with reconstruction in order to lower that risk.
- Patients who carry the BRCA2 genes have a 60% chance of developing breast cancer by age 70.
- Patients who have either gene should undergo preventive mastectomies and reconstruction.
- Rad’s preferred method of reconstruction is the DIEP flap. If there is not enough fat in the abdominal area then implants are suitable.
DIEP Flap: corrective DIEP
- Breast reconstruction is attempted by many but performed successfully by very few.
- As such many patients, who suffer breast disfigurement caused by radiation and/or prior failed surgeries, seek out Dr. Rad to perform corrective work.
- Patients who have either gene should undergo preventive mastectomies and reconstruction.
“Safety, artistry and compassion…my guiding principles.”
- Ariel N Rad, MD, PhD, FACS
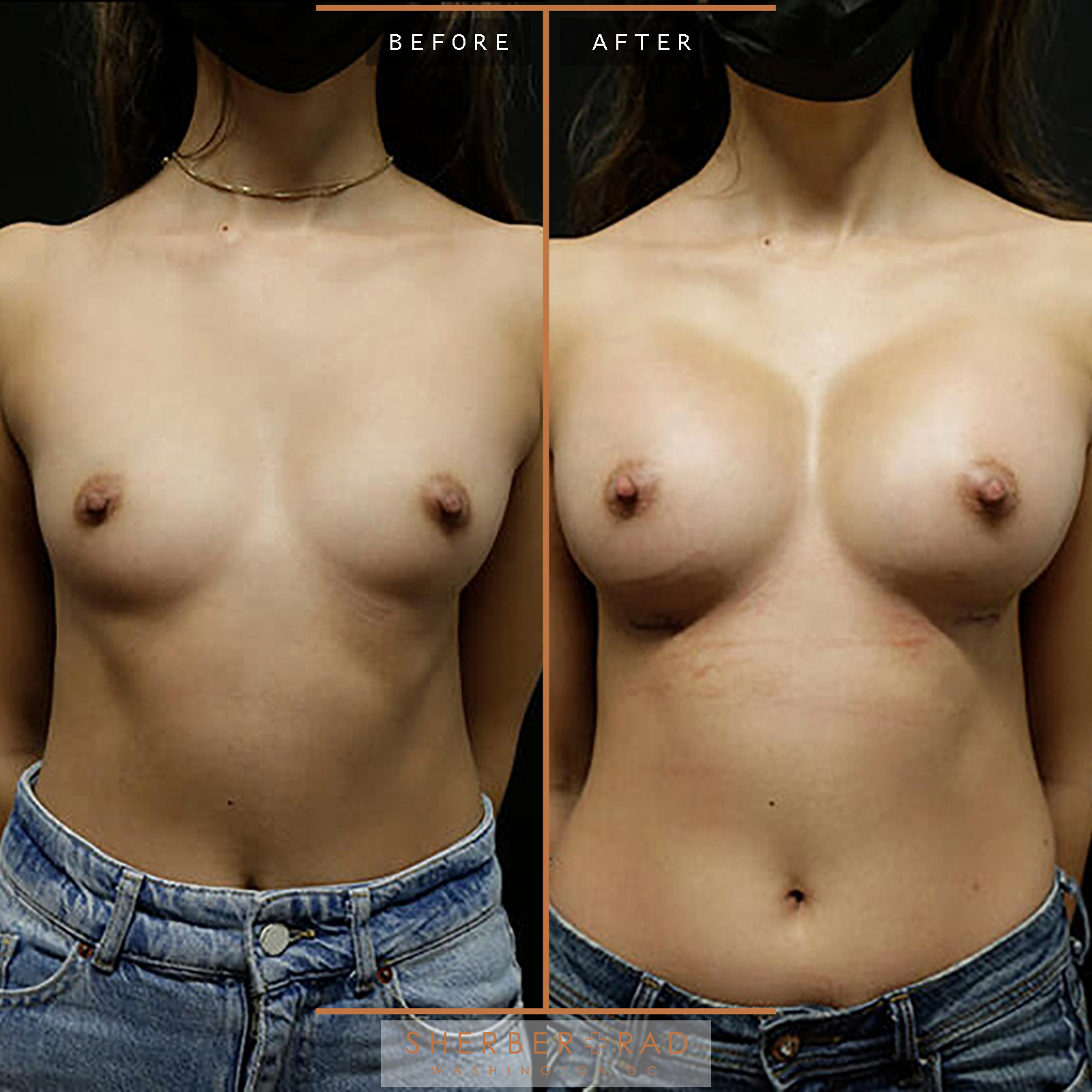
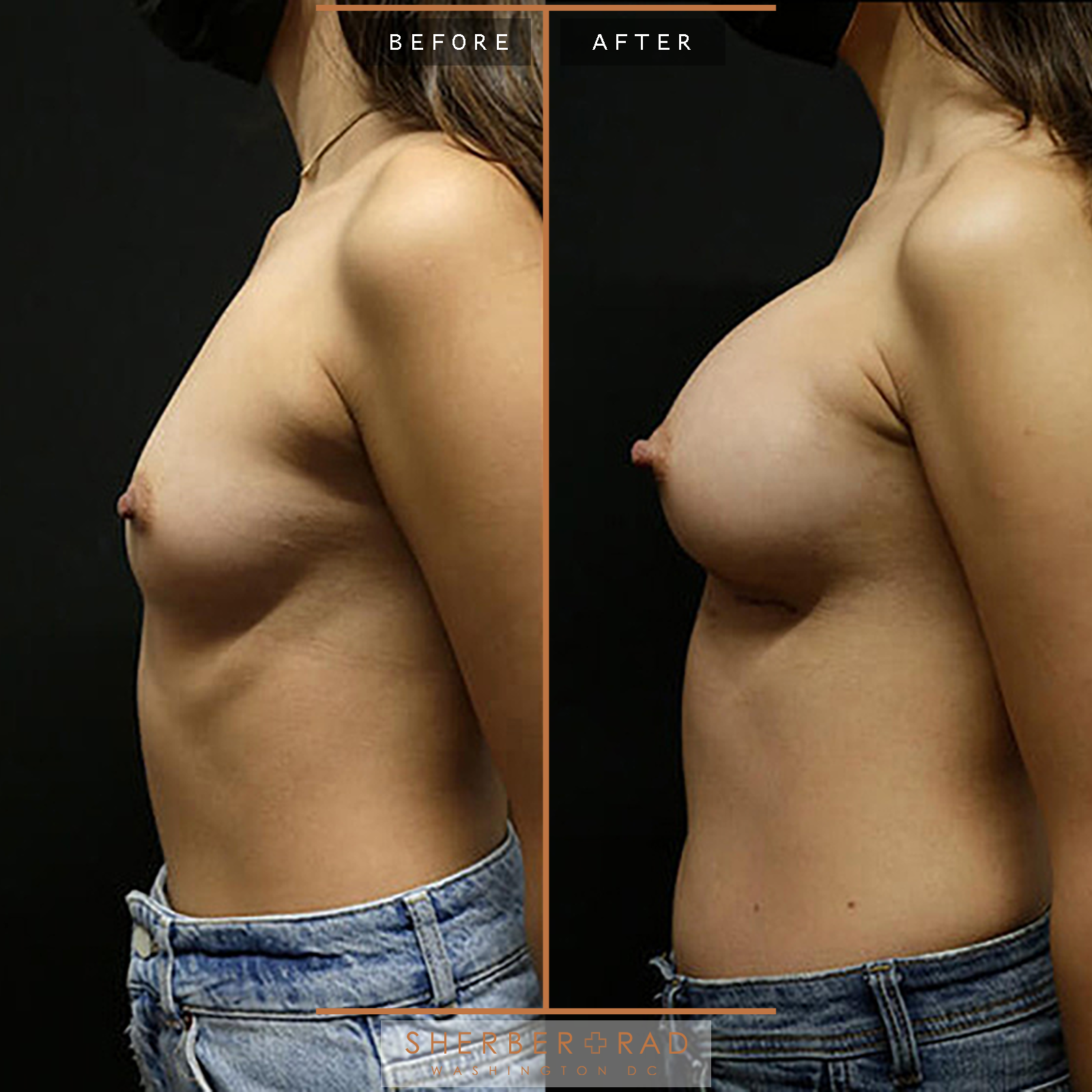
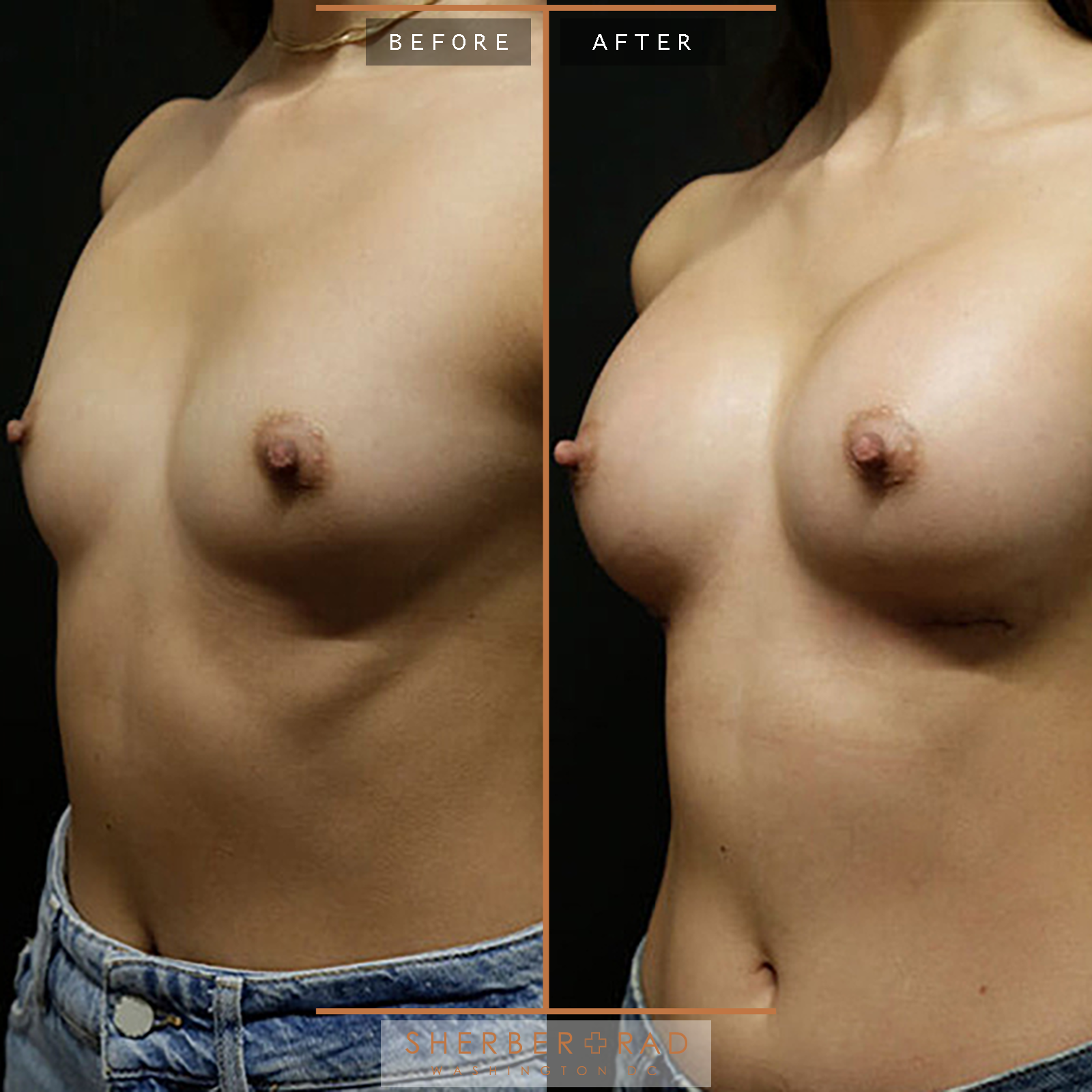
real patient resultsgallery
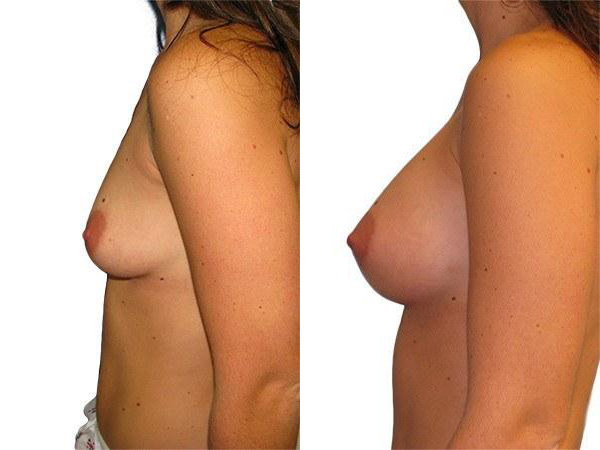
before
after
before
after
before
after
before
after
before
after
before
after
before
after
before
after
before
after
before
after
01Artistry
02safety
03Technique
04recovery
You will stay in the hospital typically 3 nights. This is to monitor the flaps and make sure that they stay healthy and to get you back to normalcy as soon as possible. While in bed immediately after surgery, you will be flexed up at the hip so that there’s minimal tension on your abdominal wound. You may have a warming blanket, and the nurse will be checking on you every hour to ensure that there is good blood flow through the flaps. You will not be given food or drink the night after surgery, but you will be well hydrated with IV fluids. The next day after surgery you’ll be moved to a chair and given liquids and your diet advanced. The 2nd day after surgery you’ll be able to walk with assistance, and you’ll be weaned off of IV medications and fluids and started on oral pain medications. The 3rd day after surgery you’ll be able to go home.
05Aftercare
Wound and drain care is straightforward (see separate wound care and drain care documents for details). Dressings will be removed by your nurse prior to discharge on day 3 after surgery. You will then shower daily, scrub incisions and drain sites, and apply Aquaphor over incisions. Perform drain care twice daily. Instructions for how to use the drains will be provided by the nurse who discharges you from the hospital.
06longevity
frequently askedQuestions
How do I know if I’m a good candidate for DIEP Flap Breast Surgery?
Most women who have experienced a whole or partial mastectomy tend to be ideal candidates for the breast reconstruction technique known as DIEP Flap. This procedure can be performed either at the same time as their initial mastectomy (immediate reconstruction) or months, even years, later (delayed reconstruction). The goal of the procedure is to provide survivors of breast cancer an opportunity to restore their breast/s which were excised during the surgery to remove cancerous cells. This procedure has brought peace of mind to thousands of cancer survivors looking to return to their normal lives.
You may be a candidate for DIEP flap procedure if:
- you are healthy
- you desire your own tissue for reconstruction
- you have extra fat in your lower abdomen
- you don’t have long abdominal scars that go across your entire abdomen
- you do not want, or cannot have implants
- want their breasts to be rebuilt with their own natural tissue
- do not have long (across the midline) scars across the abdomen from prior surgery
Even if you’ve had prior abdominal surgery such as liposuction, appendectomy, gallbladder surgery, or C-section, you are still likely to be a candidate for the DIEP flap. Keep in mind that the final determination depends on Dr. Rad’s assessment.
Patients who need, or who have had, radiation therapy are good candidates for DIEP flap reconstruction rather than implants because of internal scarring (called “capsular contracture”) often caused by radiation. In general, if you have about as much abdominal fat as your current (or pre-mastectomy) breast size, then the DIEP flap may be a good option. Even if the volume of abdominal fat is smaller than your breast size, with outpatient fat grafting procedures Dr. Rad often is able to rebuild your breast(s) to the size you desire. Dr. Rad will guide you in this decision.
What are my other options besides DIEP Flap Breast Surgery?
- Implant Reconstruction is the most popular option owing to the ease of recovery and simplicity of surgery; however, implant reconstruction often is not a good option due to scar tissue problems caused by prior breast radiation.
- LSGAP “Love Handle” Flap Reconstruction borrows love handle fat and is the most complex breast reconstructive operation in existence; Dr. Rad is 1 of only 30 microvascular surgeons worldwide who is able to perform it.
What is DIEP flap?
A DIEP flap is a type of tissue flap that borrows tissue from the abdomen and transfers it to the breast for a complete rebuild (see figure, right). It’s a highly effective tool that only plastic surgeons with specialized training in microsurgery are able to perform. Very few plastic surgeons in the world are able to do these types of flaps. The DIEP flap is an excellent option for those who need radiation treatment, because it solves problems associated with implants, such as ‘capsular contracture,’ which is a constricting scar around the implant. It also provides the most natural and permanent reconstructive option to women while also giving patients a ‘tummy tuck,’ or flat and contoured abdomen, which is a desirable outcome for patients with extra abdominal fat. It is also very unique in that it spares the abdominal “core” muscles which are important for core stability. This makes the DIEP flap very different from the TRAM flap which completely removes the core abdominal muscle(s) (in addition to the overlying skin/fat). Most plastic surgeons are unable to perform DIEP flaps due to lack of skill in microvascular surgery, and instead they offer the TRAM flap because it is easier to perform. However, there are down sides to removing the core muscles: while the TRAM flap works well for breast reconstruction, more studies are showing that the problems that removing the core muscles cause is not worth it: weakness of the core, difficult rising from bed or a chair, coughing, sneezing, and providing trunk stability; also hernias or bulges occur much 4 times more frequently with TRAM flap surgery and this often leads to surgery for repair. For this reason, Dr. Rad chose not to offer the TRAM flap.
If my insurance tells me that Dr. Rad’s care is covered then is all hope lost?
As the saying goes, “the squeaky wheel gets the oil”! You’ll need to plead your case with your insurance company which often needs reasons from you for why Dr. Rad must do your surgery as opposed to another surgeon. Insist your insurance company “I want Dr. Rad to be my surgeon because”: Dr. Rad has unique expertise in microvascular perforator flap (DIEP, SGAP) surgery Dr. Rad trained at the world’s top institutions for microvascular perforator flap surgery Dr. Rad’s flap success rate is higher than the national average (99% vs 97%) Dr. Rad’s operative times are much lower than the national average even for 2 surgeon teams (for bilateral DIEP flaps : 5.5 hours vs 8-10 hours) Dr. Rad’s complication rate is much lower than the national average Dr. Rad’s length of hospital stay is much lower than the national average (3 nights vs 4 nights) Dr. Rad’s team is highly experienced in DIEP flap surgery This “the squeaky wheel gets the oil” approach gives you the best chance of success. If they still do not agree to covering Dr. Rad then you should insist on a “peer to peer” call between the Medical Director and Dr. Rad.
Does it matter which surgeon(s) perform(s) my surgery?
Yes! This is the most important decision to make. Surgeons’ experience, training, flap success rate (and flap loss rate), operative times and rate of abdominal hernia/bulge are the most important details for successful and safe surgery. While many surgeons claim to perform the DIEP flap, there is a wide range of experience. High flap loss rates (> 5%) and long operative times (> 10 hours) can lead to complications; removal of abdominal muscle (such as in the TRAM flap) can lead to hernias and bulges which require future reconstructive surgery. For your safety go to the right surgeon regardless of insurance coverage. Dr. Rad is very transparent and honest with patients about his process. Over 10 years of practice Dr. Rad has performed well over 1,200 free perforator flap surgeries for breast reconstruction. His statistics are as follows (national averages shown in [brackets]): Over 1,200 DIEP, SGAP and TUG flaps Flap success rate: 99.2% [national average: 97%] Flap loss: 0.8% [national average: 3%] Abdominal Bulge Rate: 0.5% [national average: 5%] Hernia Rate: 0% [national average: 3%] Hematoma: 0.5% [national average: 4%] Unplanned return to OR: 2% [national average: 7%] A number of surgeons who claim to perform the DIEP flap may in fact not perform it. This may be difficult to ascertain. The best way to find out a surgeon’s track record is to ask other patients and read online patient reviews. Also, we are happy to connect you with one or more of Dr. Rad’s patients to give real accounts of their experiences.
What questions should I ask my surgeon?
Questions should zero in on a surgeon’s experience and what to expect: How many DIEP flap surgeries have you performed? (The more experience the better) What is your “flap loss rate”? (This should be no higher than 2.5%) How long is your operative time? (On average this should be less than 4 hours for unilateral, less than 8 hours for bilateral. Excessively longer OR times are usually not necessary and may indicate inexperience.) Will there be another surgeon participating in my surgery? (Two surgeon teams are usually not necessary and may speak to relative inexperience of both) What is the chance of returning to the OR to address a blood flow problem? (This should be less than 7%) Do you use mesh to reinforce the abdominal wall? (This is usually unnecessary – routine reinforcement of the abdomen usually indicates that muscle may be taken in surgery) How long will I be in the hospital? (For Dr. Rad’s patients, 99% of the time patients stay 3 nights).
If I’ve had abdominal surgery in the past, can I still have the DIEP flap?
If you have abdominal scars (aside from very small ones as from laparoscopic surgery) then Dr. Rad will advise you whether you’re a candidate for a DIEP flap. The most common scar is from a C-section – the majority of the time these scars do not pose an issue. However, in about 1% of patients, a C-section scar has cut through the blood supply to the abdominal skin/fat which makes the DIEP flap impossible to perform. You will need to have a CT Angiogram, a specialized cat scan that shows the blood vessels to the abdominal tissues. This is an excellent test to determine if you are a candidate for a DIEP flap, especially if you have scars that may be an issue. Other reasons that patients may not be a good candidate for a DIEP flap are those with a history of clotting problems such as deep venous thrombosis, pulmonary embolism, known coagulation problems, or patients with severe medical problems such as heart, lung, kidney disease.
I’ve been told that I don’t have enough abdominal tissue for the DIEP flap - do I still have options?
This is a rare situation because Dr. Rad performs the full spectrum of reconstruction and usually he can come up with a unique plan that fits your goals. If you are slender and Dr. Rad determines that the amount of abdominal tissue does not match your breast size goal, then the following are good options to achieve your goals: 1. DIEP Flap(s) [1st stage]; Liposuction Flanks and Fat Transfer [2nd stage] 2. DIEP Flap(s) + Implants [1st stage] 3. DIEP Flap(s) + TUG Flap(s) (called “stacked flaps”) [may require a 2nd stage] 4. DIEP Flap(s) + Latissimus Flap(s) (“stacked flaps”) [may require a 2nd stage] These are all excellent options and the final choice depends on your goals and Dr. Rad’s assessment of the best path forward.
Do I need any special tests before DIEP flap surgery?
A CT scan of your abdomen for pre-operative planning of the DIEP flap is necessary and will need to be done no later than 2 weeks prior to your DIEP flap surgery. The CT scan provides important information, specifically: (1) the exact location of the dominant blood vessels (this helps to decrease surgery time and optimize flap success), (2) whether C-section scars have compromised blood flow to your abdominal tissues, and (3) presence of hernias. We will provide a prescription for the CT scan. You should have this done at Fairfax Radiology – please call 703-698-4441 to arrange the appointment. Their fax is 703-698-0864. Dr. Rad will review the images and determine if the CT scan shows good blood supply making you a good candidate for DIEP flap(s).
Will I need a 2nd surgery to complete my reconstruction?
Most patients benefit from a subsequent outpatient surgery referred to as a “revision” or “touch up” procedure. Dr. Rad will discuss with you whether you would benefit from a revision. Most often after DIEP flap reconstruction patients have slight asymmetries in breast shape, surface contour and volume. Patients may also elect larger or smaller overall breast size and they need nipple reconstruction. All of these issues are addressed to achieve the most beautiful result possible. Insurance does cover revisions and recovery is much easier, lasting on average 3-7 days.
What insurance is Dr. Rad in network with?
BCBS Carefirst – individual contract, BlueChoice Advantage, BlueChoice HMO, BlueChoice HMO Open Access, BlueChoice HMO Referral, BlueChoice Opt-Out Open Access, BlueChoice Opt-Out Plus Open Access, BlueChoice Plus, BlueCross BlueShield Preferred (MSP), BluePreferred PPO, Comprehensive Major Medical, FEP – Federal Employee Program, HealthyBlue 2.0, HealthyBlue Advantage, HealthyBlue HMO, HealthyBlue Plus, HealthyBlue PPO, Maryland Point of Service (MPOS) – requires a Carefirst referral for all services rendered, Personal Comp, Traditional/Indemnity, BCBS Out of State– individual contract, Only BlueCard PPO Plans – the insurance card with have a suitcase logo with a PPO inside, Cigna – group contract, Cigna HMO, Cigna PPO, Cigna Open Access Plus (OAP), Medicare – individual contract
Will I be covered if Dr. Rad is out of network with my insurance?
Yes, and the good news is that most insurance companies recognize that Dr. Rad is one of the few surgeons with microsurgery (DIEP flap, SGAP flap, TUG flap) expertise in breast reconstruction. Therefore, if you have OON benefits then our billing department usually can convince your insurance company that Dr. Rad is the only surgeon capable of performing your surgery. Keep in mind that you must have OON benefits as part of your insurance plan to have insurance coverage. If you do not have OON benefits then you should add these to your plan, or switch to an insurance plan with which Dr. Rad is in network (see separate Q+A).
What will my out of pocket cost be under Dr. Rad’s care?
Your out of pocket cost (OOPC) is determined by your insurance plan and consists of co-payments, co-insurance and deductible. If you are unsure what your deductible/co-payment/co-insurance amounts are, call your insurance company and inquire. This information should be freely provided. If you would like us to help determine your OOPC then we can give an estimate after you consult with Dr. Rad. Call 202.517.7299 to schedule your consultation.
Testimonials